SOP
This document relates to all Physiotherapy Practitioners employed by the Ministry of Health (MoH). It is aimed at the patient, as well as clinical staff such as inpatient and outpatient to inform Physiotherapy Practitioners, nurses and doctors to provide guided evidence based quality service.
The purpose of the Physiotherapy Department is to provide an expert physiotherapy service, with systematic methods of assessing Neuromuscular-skeletal disorders of function including pain and those of a psychosomatic origin and dealing with or preventing these problems by natural methods based essentially on movement, manual therapy and physical agencies. This pack helps guide the patient, and Physiotherapy Practitioner from their pre – op stage (physiotherapy prior to operation), their inpatient stay, and then their post-operative outpatient physiotherapy stage.
Physiotherapy departments must adhere to a very high level of standards. A description of such standard measures is included as follows:
This document relates to all Physiotherapy Practitioners employed by the Ministry of Health (MoH). It is aimed at the patient, as well as clinical staff such as inpatient and outpatient Physiotherapy Practitioners, nurses and doctors to provide guided evidence based quality service.
The purpose of the Physiotherapy Department is to provide an expert physiotherapy service, with systematic methods of assessing musculo-skeletal disorders of function including pain and those of a psychosomatic origin and dealing with or preventing these problems by natural methods based essentially on movement, manual therapy and physical agencies. This pack helps guide the patient, and Physiotherapy Practitioner from their pre – op stage (physiotherapy prior to operation), their inpatient stay, and then their post-operative outpatient physiotherapy stage. The aim of this document is to help improve management of both cumulative and traumatic orthopedic conditionsby improving the quality of rehabilitative care and reducing risk.
Rehabilitation following the initial injury and prior to surgery is very important to aid recovery back to health and to meet goals. Goals could include:
An initial assessment of every patient will be entered by a Physiotherapy Practitioner in the patients’ case sheet, for inpatient initial assessment must be recorded in the patient’s file. Initial assessment will include information gathered by the Physiotherapy Practitioner as follows:
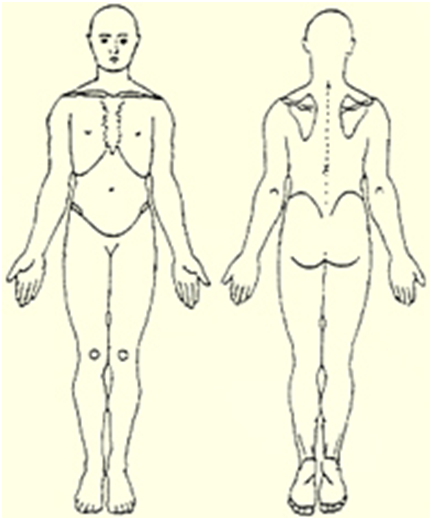
The main problem is usually recorded on a body chart, all which have similar features & all are similarly asexual. The chart on the left is a more or less standard view of one. It shows an anterior & posterior view of the body & shows it in the anatomical position. Some departments will have their own symbols for describing pain, stiffness, acute, chronic, whether it radiates, etc.
(Medical Council 1976)
| Grade | Muscle Activity |
|---|---|
| 0 | No contraction |
| 1 | Flicker or trace of contraction |
| 2 | Active movement with gravity eliminated |
| 3 | Active movement against gravity |
| 4 | Active movement against gravity and resistance |
| 5 | Normal strength |
Refers to eliciting of deep tendon reflexes by tapping the tendon a number of times, commonly used deep tendon reflexes are the biceps, triceps, patellar &tendo-calcaneus. These reflexes may be graded as follows:
| 0: Absent | Areflexia |
| 1: Diminished | Hypoflexia |
| + or 2: Average | Normoreflexia |
| ++ or 3: Exaggerated | Hyperflexia |
| +++ or 4: Clonus | Clonus |
Cyriax (1982)
Tests the Neurological integrity of the NS, usually to establish effects of compression of the PNS and these tests include Neurodynamic testing & some other tests.
Effects of compression of the PNS are:
Then the following information is noted:
Date of examination: File number:
Name: Age: Gender:
Address: Phone: Email:
Occupation:
Blood Pressure:
Temperature:
Heart rate:
Pulse rate:
Respiratory rate:
Case History
Dyspnea [ ]
Orthopnoea [ ]
Wheeze [ ]
Cough [ ]
Sputum [ ]
Pain [ ]
Operations [ ]
Accidents [ ]
Rheumatic fever [ ]
Pulmonary TB [ ]
TB Contact [ ]
Known Allergy [ ]
Others: (Specify)
Current drugs:
Married [ ]
Single [ ]
Widow [ ]
Widower [ ]
Divorced [ ]
Drinks alcohol [ ]
Smokes [ ]
Hobbies:
Gait:
Posture:
Anemia [ ]
Cyanosis [ ]
Clubbing [ ]
Edema [ ]
Pectus Carinatum [ ]
Pectus Excavatum [ ]
Acquired:Scoliosis [ ]
Kyphosis [ ]
Barrel Chest [ ]
Cervical Spine Mobility:
Thoracic Spine Mobility:
Shoulder girdle Mobility:
Primary:
Accessory:
Upper costal [ ]
Lower costal [ ]
Thoracic [ ]
Abdominal [ ]
Chest Radiograph:
Pulmonary Function Test (Spirometry):
Exercise tolerance (number of stairs client can climb or distance client can walk)
Note: The Essence of auscultation is to determine air entry and detect possible abnormal sounds associated with breathing.
Summary of Findings:
Aims/Objectives for intervention:
Plan of Intervention/Management:
Short Term:
Long term:
Name of Physiotherapy personnel:
Date for Re-examination:
UTH protocol
Neurological physiotherapy is a program specializing on patients with trauma, diseases or disorders of the nervous system. Our goal is to reduce symptoms, and improve the well-being of the patient. We try to satisfy the needs of every single patient in our neurological physiotherapy program. The success of the physiotherapy however, doesn't only depend on the doctor, but also on the patient and their family.
The neurological rehabilitation focuses on physiotherapy for adults and children suffering from various diseases and conditions such as vertebra-genic disorders, neurological diseases, patients after surgeries, injuries of locomotive system, spine surgeries, as well as, patients with internal diseases that affect either peripheral or central nervous function.
Other prerequisite necessary for success is a variation of aids and devices. From orthotic aids, splints to complex instruments designed with the principle of biofeedback.
The patient is being scheduled for evaluation by physiotherapy practitioner as soon as possible. After evaluation the therapist must explain the plan of treatment to the patient.
Assessment by physiotherapy practitioner includes subjective, objective assessment and testing to determine suitability for further referral – history of present condition, past medical history, social history, drug history, special condition/area related questions, and goals at problems.
Objective assessment includes visualisation of the patient, their posture or gait, side and state of paralysis, Range and level of functional performance testing and special neurological tests.
A neurological rehabilitation program is designed to meet the needs of the individual patient, depending on the specific problem or disease. The goal of neurological rehabilitation is to help the patient return to the highest level of function and independence possible, while improving the overall quality of life — physically, emotionally, and socially.
In order to help reach these goals, neurological rehabilitation programs may include the following:
Some disorders of the inner ear result from the displacement of very small granular material from where they normally reside [within the vestibule] to other areas [semicircular canals], causing vertigo and imbalance. These symptoms can be very disabling, brought on by certain commonly performed movements such as turning in bed, looking up or turning one’s head. Physiotherapy practitioners, who have specific training, can employ specialized techniques [Canalith Repositioning Procedures; CRP] to return these tiny granules to their correct resting place, resolving this type of positional vertigo. The treatment is quick, painless and highly effective, within the first ten sessions.
Analyze the body’s posture to identify areas of imbalance and inordinate stress, which are possibly contributing to a person’s chronic pain or functional impairment. We use corrective measures to restore proper alignment of the musculoskeletal system to reduce undue stress and strain.
Assessment of:
Physiotherapy practitioners are trained to understand proper movement techniques to:
Retraining of:
This is a highly specialized form of therapeutic exercise and movement re-training that often involves detailed exercise testing to guide and evaluate treatment and the use of visual biofeedback techniques in order to enhance the effects of therapy
Analysis of the different stages of walking to determine any deviations and the training to re-educate the body in the proper movement patterns:
Exercises and activities to improve the ability to maintain the body in equilibrium
Exercise is a very common and non-invasive method of treatment used in a physiotherapy setting. Exercise can help to improve patients:
The uses, categories and variations of therapeutic exercise are too numerous to be presented in any detail here. However, very generally, they can be:
Physiotherapy practitioner will determine which exercises are appropriate for the patient and in which way to start and progress or change them. Exercise is almost always incorporated into a physiotherapy program, and usually involves activities that the patient will be instructed to perform at home on their own, in addition to the clinical setting with a therapist.
Neurological physiotherapy session may last anywhere from 45 minutes to 90 minutes depending on the severity of patient's condition.
The physical changes to a women’s body as related to pregnancy are multiple. The centre of mass changes, there is more pressure on the organs, and there is increased weight to be carried. All of this in a relatively short span of time often leads to back pain, pelvic pain and urinary incontinence. Evidence shows that group training programs designed and delivered by Physiotherapy Practitioners can relieve lower back pain, pelvic pain and urinary incontinence in pregnant women.
Physiotherapy Practitionerled exercises at 60 minutes a week from the 20th through the 36th week of pregnancy reduces the occurrence of lumbar-pelvic pain during pregnancy and after delivery.
With respect to pregnant women, it is recommended that:
While pre and post-natal exercise programs are common, and they help many mothers, they may be harming others. Therefore it is important that the following are observed:
It is within the scope of practice of a Physiotherapy Practitioner to properly:
A good Physiotherapy Practitioner delivered program for pregnant women would;
The goal of such a program would be to offer women improved
Babies that go to full-term in the womb simulate their in vivo position by keeping their limbs tucked close to their bodies for several weeks after their birth. Their brains have developed enough to keep their muscles in this flexed position, which builds strength and enables them to calm and soothe themselves.
Premature babies, on the other hand, lack the development to hold their limbs close. This approach sees Physiotherapy Practitioners:
Babies will be tested:
As a result of therapy sessions including:
Measurements will be taken at their gestational ages of 34 and 40 weeks, to indicate how to better structure physical therapy interventions.
Physiotherapy Practitioner, or physical therapist, is a health care professional that provides physical rehabilitation and pain relief to people including those with osteoarthritis, repetitive strain injury, whiplash, sports injuries, or spinal cord injuries. Paediatric therapists are increasingly trained to consider the needs of the child within the overall family structure, and encourage parents and health professionals to form partnerships around goal setting and decision making. Physiotherapy Practitioners work closely with families, carers, teachers, doctors and other health professionals. The approach is holistic and practical, with an emphasis on gross motor function and posture.
Paediatric Physiotherapy Practitioners work with people of varying ages from premature babies to adolescents to ensure optimal physical function and development. Like all Physiotherapy Practitioners, they are concerned with movement, co-ordination, posture and the cardiorespiratory system. Treatment may involve soft tissue massage, mobilisation, stretching, specific therapeutic exercises and posture education. PaediatricPhysiotherapy Practitioners have a duty to maintain their clinical reasoning skills and up to date knowledge within their specific area of practice to ensure that interventions are appropriate and effective. Continuing professional development (CPD) to increase specialist knowledge, skill and experience can be gained through clinical working with children, attending specialist courses, reviewing the evidence base, reflecting on practice and undertaking research and is a ‘life long’ experience for all Physiotherapy Practitioners.
Standard operating procedures are a specific set of practices that are required to be initiated and followed when specific circumstances arise. In present day medicine, clinicians are familiar with SOPs in restricted contexts, such as those described at the beginning of this article. Putting in place SOPs would enable clinical practitioners manage patients effectively and efficiently. Clinical guidelines are developed using evidence-based medicine criteria and consist of two distinct components: the evidence summary and the detailed instructions for the application of that evidence to patient care. For the common health care provider, guidelines require local adaptation to suit local circumstances and to achieve a feeling of ownership, both of which are important factors in guideline uptake and use.
Therapy begins with an evaluation and assessment.
Four major areas of paediatric physiotherapy include musculoskeletal disorders, neurological disorders, oncology and cardio-pulmonary disorders. The conditions under each area are as follows:
Assessments are always made up of two parts namely the subjective and the objective. The former involves information gathered by questioning and the latter is what is seen and/or measured by the clinician. Without an accurate assessment it is impossible to develop an appropriate plan of treatment. Equally, a sound theoretical knowledge is required to develop an appropriate treatment plan for those problems which may be improved by physiotherapy. Once treatment has commenced it is important to assess its effectiveness regularly in relation to both the problems and goals (Pryor & Prasad, 2008).
Subjective assessment: Subjective assessment is based on an interview with the patient. It should generally start with open-ended questions - What is the main problem? What troubles you most? It allows the patient to discuss the problems that are most important to him at that time. As the interview progresses, questioning may become more focused on those important features that need clarification (Pryor & Prasad, 2008).
Paediatric neurological conditions include the following: Cerebral palsy; Brain injury; CNS infections leading to neurological sequelae; Complications of sickle cell anaemia (E.g. Hemiplegia); Spina bifida; Erb’s palsy; Hydrocephalus; Progressive neuromuscular disorders (Muscular dystrophies and atrophies); Hypertonia; Hypotonia (E.g. congenital Hypotonia and Acute Flaccid Paralysis); Gross Motor delay (e.g. in Down’s Syndrome); Developmental Coordination Disorder; Autism; Attention Deficit Hyperactivity Disorder; Global development delay.
| Demographic characteristics | ||
|---|---|---|
| Child’s name | ||
| Date of birth | Gender M/F | |
| Mother’s name | ||
| Father’s name | ||
| Caregiver’s name * | ||
| Phone No. | ||
| Address | ||
| Diagnosis | ||
| Classification if diagnosis is cerebral palsy |
| |
| Gross Motor Function Classification System (GMFCS)if diagnosis is cerebral palsy |
| |
| Subjective assessment | ||
| Associated Problems: | Vision, hearing, speech, epilepsy, Learning impairments, behavioural, etc | |
| Obstetric history | ||
| Before Pregnancy | ||
| During Pregnancy | ||
| Labour and delivery | ||
| Child’s birth |
| |
| Child’s case history and past medical history | ||
| Child social history | interests, motivation, cognition, ability to communicate, behaviour, social interaction | |
| Family social history |
| |
| Parents/Guardian’s main concerns | ||
| Communication: (How child communicates) | ||
| Activities of Daily Living (dependent, assisted, independent) |
| |
| Equipment: (Has, ordered, does not have, does not need) |
| |
| Referral required | ||
| Objective Assessment | ||
Physical examination Observation of child in different positions. Patterns of posture and movement (Brief description of the predominant postural patterns and movements, distribution of abnormal tone, asymmetries and associated reactions, head/trunk control and activities in upper and lower limbs) |
| |
| Hand function | ||
| Summary of predominant postural tone and patterns | ||
| Functional abilities: (What activities is the child able to do?) | ||
| Functional Limitations: (what activities is the child unable to do?) | ||
| Contractures/ Deformities | ||
| Summary of main problems | ||
| Treatment/therapy intervention | ||
| Treatment goals: ( to address main problems | ||
| Treatment Plan: (Therapy Strategies) | ||
| Home program: | ||
Musculoskeletal physiotherapy (MSK) is probably the largest area of physiotherapy in terms of practitioner and patient numbers. Paediatric musculoskeletal conditions include the following:
Respiratory care in small children is very different from that in adults. There are anatomical and physiological differences which mean that additional criteria need to be used for assessment and treatment. In management of paediatric patients, it is important to include:
Paediatric cardiopulmonary conditions managementinclude the following:
In assessment of paediatric respiratory conditions, most of the aspects are similar to adult assessment. Below are the areas that should be considered in paediatrics besides the generic assessment (From Pryor & Prasad, 2008):
Initial assessment
Medical notes: Information can be extracted from the medical notes relating to present condition and past medical history etc.
When assessing a neonate, the following points are relevant:
Examination:
Clinical signs: Normal values for heart rate, respiratory rate and blood pressure in table 2.
Table 2. Normal values of heart rate, respiratory rate and blood pressure according to age (Adapted from Pryor & Prasad, 2008).
| Age group | Heart rate (Beats/min) | Respiratory rate(Breaths/min) | Blood pressure (mmHg) |
|---|---|---|---|
| Preterm infants | 120-140 | 40-60 | 70/40 |
| Full term infants | 100-140 | 30-40 | 80/40 |
| 1-4 years | 80-120 | 25-30 | 100/65 |
| Adolescents | 60-80 | 15-20 | 115/60 |
Check for signs of respiratory distress such as:
Cardiac signs:
*Precautions for chest percussions:
Physiotherapy in paediatric oncology includes the following: